Prioritizing communication in healthcare is vital to sharing information, solving problems, navigating relationships, and negotiating differences. In a healthcare setting, communication is one of the most important tools medical practitioners have in their arsenal. Having effective communication between medical providers and patients is essential in maintaining a patient’s health.
Doctors communicate with patients to gather vital facts that are used to determine a diagnosis and formulate a treatment plan. Without that initial conversation, doctors will be left without the information they need to help them make an educated diagnosis. Continuing that dialogue once a patient heads home decreases the likelihood of them needing secondary treatment or a return trip to the hospital.
Staff members also need effective communication skills. Doctors must communicate with nurses, who are often the primary contact with patients. Hospital administrators and support staff must also be a part of the conversation.
Patient communication in healthcare is a component of every successful treatment effort and occurs during every step of the healthcare process. Studies consistently show that patients fare better when their doctors are skilled communicators.
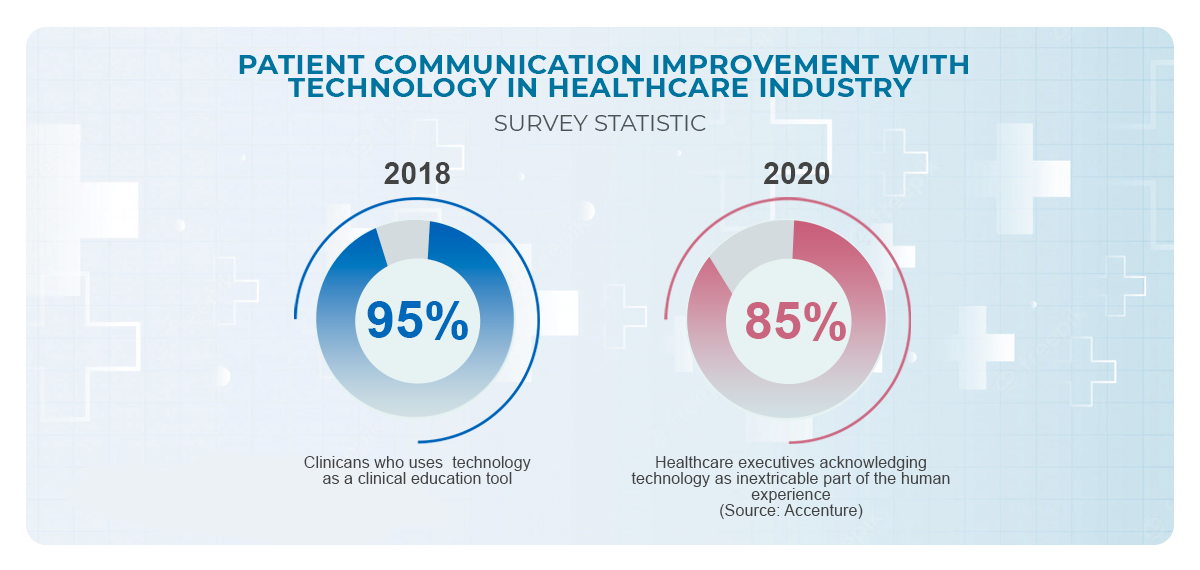
The last few decades have seen a transformation in the way medical practitioners use health tech to improve communication.
This article will discuss how important effective communication in healthcare settings is and offers tips on how medical providers can improve those skills. We will also investigate how technology is improving the way medical practitioners communicate with their patients and with each other.
Patient Communication Improved By Tech

- Diagnosis Systems
- Imaging and Diagnostics
- Mobile Health Solutions
- Telemedicine
- Electronic Prescriptions
- Appointment Scheduling
- Medical Device Software
- Equipment Management
- Hospital Management
- Medical Research
Focus on the Follow-Ups
Focusing on patient communication in healthcare shouldn’t stop once the patient heads home. Whether after a routine visit with a family doctor or an extended hospital stay, health outcomes are best when lines of communication remain open after a visit.
This is especially true when a patient suffers from a chronic condition that requires ongoing care, like diabetes or heart disease. It’s also vital for patients that require ongoing treatment, medications, or follow-up appointments. In actuality, every patient will benefit from continued conversations with medical providers.
One study showed that heart failure patients who received a follow-up call from care providers within one week of discharge from a hospital were 19% less likely to experience readmission in the next 30 days.
A similar study found that follow-up communication and care coordination increased positive outcomes for patients with diabetes. Another study showed that follow-up care after initiating a new medication improves patients’ understanding of dosing, risks, and potential side effects.
Ways to Increase Follow-up Communication
Staying in contact with patients is just one aspect of follow-up care. Ensuring patients have the knowledge and understanding necessary to maintain treatment plans and develop healthy habits will help them recover faster and stay healthy.
Telehealth
Utilizing technology to increase follow-up communication has become easier and more accessible for medical professionals and patients. Telehealth visits allow patients direct access to doctors without the need to revisit offices or hospitals.
Online Portals
Direct messaging with care teams allows patients to reach out with questions or concerns without needing an appointment. Medication questions, refill requests, and appointment scheduling can be integrated into a single digital platform. These portals also allow physicians to reach out to patients and check on their well-being, ensure follow-up appointments are scheduled, and inform patients of any information pertinent to their care.
Transportation Assistance
One of the biggest hurdles many patients face is access to transportation. Many medical facilities work with state and federal insurance companies to provide safe and accessible transportation to doctor’s appointments.
Some facilities even have partnerships with ride-sharing services to get patients to their appointments.
Automate the Process
Health technology has made it easier for doctors to follow up with patients. Automatic appointment reminders, either through text messaging, email, or automated phone calls will allow medical facilities to prompt patients to schedule follow-ups and remind them when it’s time to show up. Missed appointments can trigger a follow-up call reminding patients of the importance of follow-up care.
Start the Process Early
One of the most important conversations that occur in any medical setting is the very last one – directly before patients walk through the door and go back to their daily lives. Medical providers are responsible for ensuring patients understand every aspect of their condition, treatment plan, and ongoing care.
Communication and patient education can continue after the patient leaves a facility if the care team provides information and access to the right resources. There’s a direct correlation between a lack of understanding and non-compliance, and it’s the care team’s job to break this trend.
Be Empathetic and Humble
Doctors and nurses are extremely busy. Patient counts and workloads are increasing. It’s likely that every minute of a shift is filled with constant demands on their attention.
Medical practitioners who have been in their positions for a long time may become desensitized to the needs and anxieties of patients. They may feel like they’re effective communicators, when in reality, patients may feel confused, uninformed, and uneasy.
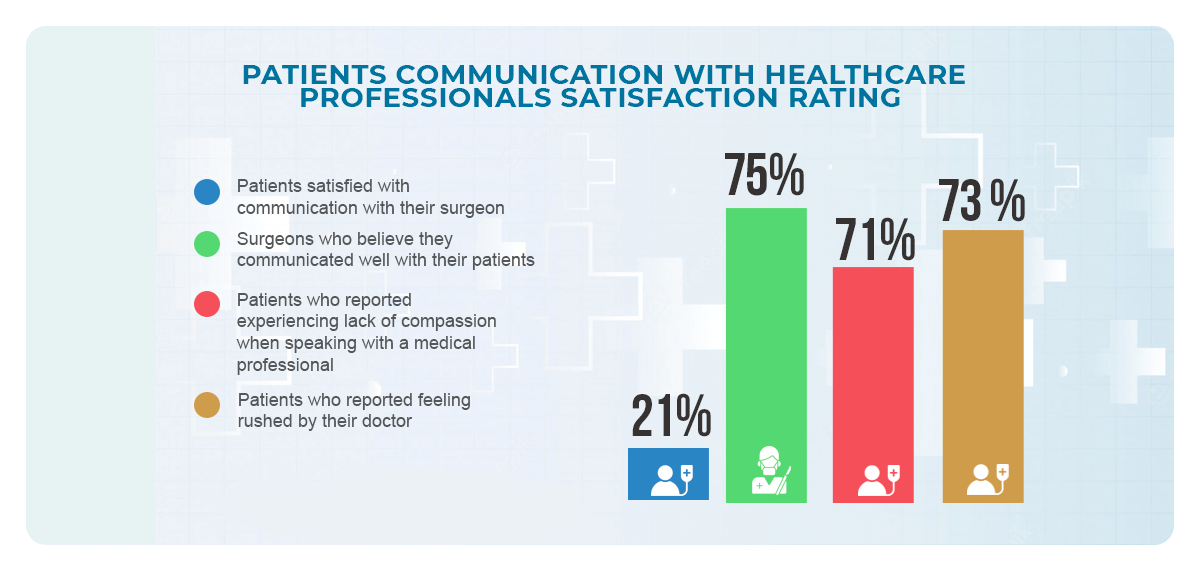
As an example, one study found that only 21% of patients felt communication with their surgeon was satisfactory, while 75% of surgeons believed they communicated well with their patients. Another survey found that 71% of patients report experiencing a lack of compassion when speaking with a medical professional and 73% report feeling rushed by their doctor. For patients, these are not positive feelings.
So what are the tools healthcare teams can use to increase their compassion and empathy? Health tech systems are a good start because they are designed to streamline processes and can free up valuable time that will be better spent with patients instead of pouring over paperwork.
Custom healthcare software systems can also delegate patient care to the right person. An entire care team can be scheduled around the needs of the patient and the organization so that each patient receives the very best, individualized care and attention.
Be Compassionate
Remember that patients are people and often may be experiencing one of their worst days. Showing compassion and understanding for their fears, anxieties, and frustrations might open the door to an effective conversation.
Build Rapport
Speak to patients as equals instead of taking a purely authoritative approach. When patients feel a sense of ease communicating with their care team, they will be more forthcoming with important information and critical details that can lead to a more accurate diagnosis.
Build Trust
Care teams can build trust with patients by being upfront, honest, and concise. Follow-through is also extremely important.
Consider Communication Barriers
Be sure to acknowledge common causes of poor communication such as differing demographics, languages, cultures, and regions.
Use the ICE Method
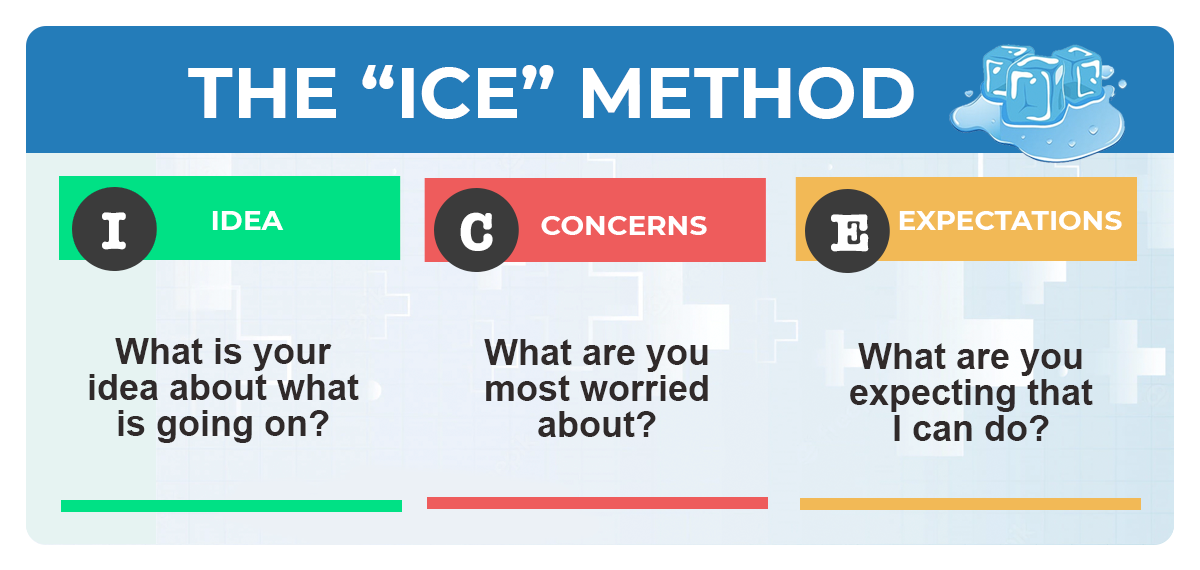 ICE stands for Idea, Concerns, and Expectations. The ICE method is a series of three questions that medical practitioners can use to facilitate an effective conversation with patients.
ICE stands for Idea, Concerns, and Expectations. The ICE method is a series of three questions that medical practitioners can use to facilitate an effective conversation with patients.
The answers to these three questions will give healthcare teams a clear understanding of what the patient believes is the problem, what the patient is concerned about, and what the patient expects in terms of care.
This information helps the medical team improve patient communication in healthcare by allowing patients the time and space to explore their feelings instead of just rattling off a list of symptoms.
Ask Open-Ended Questions and Listen
Listening is a key component of communication. Doctors not only need to communicate with their patients, but they also need to listen to what their patients have to say. Patients are the biggest, and often only, source of information medical teams have at their disposal.
 Making sure patients understand every detail about their diagnosis and care increases the quality of that care and reduces the risk of catastrophic error.
Making sure patients understand every detail about their diagnosis and care increases the quality of that care and reduces the risk of catastrophic error.
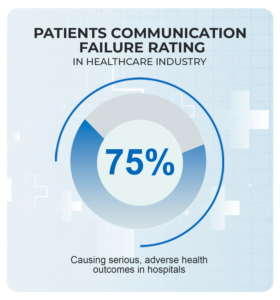
One study found that communication failure was the cause of over 70% of serious, adverse health outcomes in hospitals.
The same study found that two out of three patients leave the hospital not knowing their diagnosis and 60% leave a doctor’s visit unclear about medication or follow-up instructions.
Asking open-ended questions is one way to increase patient communication in healthcare. Open-ended questions prompt the patient to provide details and explanations rather than offering a simple yes or no answer.
The ICE method uses examples of open-ended questions. Instead of asking the patient, “do you have any concerns,” an open-ended question would be, “what concerns do you have?” The simple change in phrasing encourages patients to consider their responses instead of quickly answering with a single word.
Use Active Listening
Give the patient your full attention while they’re speaking. That means facing them directly, maintaining eye contact, and fighting the urge to interrupt. It’s also wise to avoid updating charts while the patient is speaking so they don’t feel like you’re not listening.
Implement Teach-Back Methods
Teach-back is a technique where doctors explain something to a patient and then ask the patient to explain it back to them. This method replaces the typical doctor-patient question of “do you understand.” While patients may believe they understood a conversation, the teach-back method asks them to repeat information to ensure they understood and will be able to retain the information correctly.
Use Positive Words and Avoid Medical Terminology
An increasing focus on the importance of patient communication in healthcare has created the need for all medical providers to be skilled communicators. With health outcomes closely tied to positive and effective communication, doctors and nurses can no longer rely on the off-chance that their innate skills will be enough – they must actively work to improve their communication methods.
Below are some ways medical providers can use effective communication techniques to increase patients’ understanding.

Speak in simple terms – Speak in clear, simple terms that the patient can understand. Avoid using complex medical terminology that will leave patients confused and anxious.
Focus on patient-centered communication – Patient-centered communication describes how medical providers should communicate with patients. In essence, it means meeting patients where they are – and matching terminology to best benefit their comprehension.
Consider the patient’s perspective – Remember that patients don’t have the same background, education, and experiences as those in the medical profession. Speak in a manner that will aid their understanding instead of hampering it.
Use positive language – Positive language will ease patients’ concerns and help them feel more at ease. Not every healthcare scenario will have a positive outcome, so this task may always be as easy as it sounds. The key is to use empathy and compassion and reframe the situation to focus on positivity instead of offering doom and gloom.
Be transparent – Honesty and openness in every response and conversation are vital. Don’t withhold information from a patient because you’re afraid to upset them. Doing so will only lessen their understanding and decrease their level of care. Instead, aim to offer the truth in an empathetic way.
Use visual aids – Research shows that using a combination of spoken language and visual aids can help patients understand and retain information. Many people learn better through visual input than by simply listening to an explanation.
Nonverbal Communication is just as Important as Verbal
Let’s examine two hypothetical situations. In the first scenario, a patient gets a visit from a doctor. They have probably had to wait for some time and are feeling anxious.
The doctor enters the room briskly, fails to make eye contact for more than a few seconds, spends a significant amount of time staring at the ceiling, and then breezes out of the room in less than five minutes. Our patient is left feeling unimportant and with a list of unanswered questions.
In the second scenario, the doctor enters the room and greets the patient, using direct eye contact, a disarming smile, and a calm voice. The doctor listens to the patient’s concerns, answers any questions, and ensures the patient understands every detail, maintaining attention on the patient throughout the entire conversation. Before leaving, the doctor assures the patient that the care team will take every possible step to help the patient recover.
Which scenario is likely to create the best environment for quality care and recovery – the doctor who gave the impression they couldn’t be bothered beyond the required five-minute visit or the doctor who showed compassion and empathy?
Body language is a powerful tool for patient communication in healthcare, even when we don’t recognize it. People engage in body language “habits” that are more subconscious than conscious. They may not even realize how their nonverbal cues affect another person.
Patients look to medical providers for answers, explanations, and compassion. Sending the wrong signals with unintentional body language is likely to make patients feel disregarded, and send a negative message that will resonate with the quality of care.
Take a look at this list of non-verbal cues, and then consider how it would make you feel as a patient if your doctor was doing any of them in front of you.
- Tapping fingers impatiently
- Gazing around the room
- Yawning
- Looking at a watch
- Checking a phone
- Standing over someone
- Crossing their arms
- Shaking their head
- Rolling their eyes
While avoiding these behaviors may seem like common sense, it’s easy to accidentally slip them into a conversation, especially after a long day of visits and consultations. Be aware of your body language from the moment you enter a room until the final handshake (or fist bump) so you don’t accidentally come off as callous or disinterested.
Positive non-verbal cues can create an entirely different environment. Even sitting during a conversation instead of standing can make a patient feel more comfortable. Lean forward slightly and nod your head to show you are actively listening. Maintain meaningful eye contact, smile when appropriate, and stay relaxed but engaged.
Nurses are Essential in Patient Communication
Most people, both inside and outside of the healthcare industry, understand that nurses are the backbone of a care team. On average, registered nurses and nurse practitioners see three or more patients every hour in a medical facility. Nurses are often at the front of patient care – they are the first ones into the room and the last ones out before a patient leaves.
Not only are nurses one of the most important facilitators of patient communication in healthcare, but they are tasked with sharing vital information with doctors and other medical professionals. Doctors look to nurses to keep them up-to-date on a patient’s current condition, needs, and concerns. They are responsible for administering medication, ensuring patients are cared for and safe, and orchestrating daily care tasks.
Nurses must be effective communicators because patients’ health and well-being rely on their actions. The risk of medical errors, which can be life-threatening or even deadly, is greatly increased when communication is lacking.
A study conducted by CRICO Strategies found that out of 23,000 medical malpractice lawsuits, 7,000 resulted from communication errors, and around 2,000 patient deaths resulted from those failures.
The amount of communication passing between patients and nurses – and nurses and doctors – dictates that nurses have good communication skills. Below is a sampling of the skills nurses can use to facilitate effective conversations and communication during every interaction.
- Speak with precision when communicating
- Use kindness, compassion, and empathy to generate positive relationships
- Respect a patient and their family in every instance
- Use written notes to limit misunderstandings
- Maintain accurate records
- Employ active listening skills
- Be sensitive to cultural differences
- Pay attention to personal body language
- Be aware of patient cues, both verbal and non-verbal
- Utilize healthcare technology to assist in communication
Benefits of Good Patient Communication

The use of custom software systems helps healthcare facilities streamline processes, save time on repetitive tasks, consolidate information for easy access, and monitor every aspect of their organization.
But for many doctors, nurses, and administrators, the biggest benefit is an increase in their ability to provide focused, quality care and improve communication with patients. Effective patient communication in healthcare is one of the biggest drivers of successful outcomes and gives patients the very best chance at making informed decisions about their ongoing care moving forward.
Builds Meaningful Relationships
Communication fosters relationships in every setting. The type of relationship is highly dependent on the situation in which the conversation takes place – and a particular kind of communication works best in a healthcare setting. But the fact is, improved doctor-patient relationships increase the chances of a positive outcome for both parties.
Increases Patient Satisfaction
Patients who are satisfied with a healthcare encounter are more likely to be active participants in their care. High satisfaction rates also increase the likelihood that patients will return for follow-up care.
Decreases Patient Readmissions
Improved communication increases a patient’s understanding of treatment plans and their responsibilities regarding follow-up care. They are less likely to make mistakes, disregard instructions, or use medication incorrectly because they understand every detail before leaving the hospital or doctor’s office.
Benefits Quality of Care
Increased communication means that medical providers and care teams can access every bit of information patients can provide. Having access to that information aids diagnosis and helps care teams create an effective treatment plan. It increases the quality of care received because patients can communicate their needs and concerns to their care team openly.
Facilitates Internal Cooperation
Communication is important in any professional setting, including medical facilities. But the importance in these settings is magnified because patients’ health, well-being, and even their lives are at stake.
Reduces Costly Errors
Mistakes in a medical setting can range from minor to deadly. Improved communication, and the use of technology to create more effective patient communication in healthcare, reduce the risk of errors and will save lives.
Poor Patient Communication and Common Mistakes
When communication between doctor and patient suffers, a patient’s well-being suffers also. And communication between doctors and nurses is just as important, if not more so. Even communication between individual providers is vital. There is no relationship in a medical setting that doesn’t feel the negative consequences of poor communication.
Poor communication can lead to a long list of negative results in a healthcare setting, such as:
- A lack of understanding and comprehension between individuals
- Increased wait times
- Decreased patient satisfaction
- Inaccurate or incomplete diagnoses
- Poor or incorrect treatment plans
- Unclear instructions
- Medical mistakes
- Increased readmission rates
- Unnecessary visits
- Additional paperwork
- Ineffective policies
- Technical Issues and errors
- Scheduling errors
- Conflicts and misunderstandings
Common Mistakes in Communication in Healthcare
Patient communication in healthcare is a skill that everyone working in a healthcare setting must develop, like all skills, performing it successfully and consistently takes practice and work. Mistakes made along the way are almost guaranteed but can be a learning tool to improve outcomes in the future.
Communication between a doctor and patient is fully the responsibility of the medical provider. A common mistake when dealing with doctor-patient communication is a lack of attention and care given to the patient by the doctor. Allowing conversations to feel rushed and incomplete is certain to lead to mistrust from the patient and will damage the relationship forever after.
Another mistake doctors make is not taking the time to ensure the patient comprehends everything without question and then taking the time to answer questions concisely and thoroughly. Doctors and patients must be care partners, and each party must always understand the other.
Final Thoughts…
The fields of medicine and healthcare are constantly evolving and the past few decades have seen an explosion of progress. It’s often said that struggle spurs progress. That has certainly been true in the healthcare sector recently.
The percentage of healthcare facilities using custom healthcare software was growing before Covid-19 ramped up in 2020. Patients are accessing and using healthcare services differently, often utilizing telehealth services, automated appointment reminders, medication reminders, and even reading over their medical charts from their mobile phones.
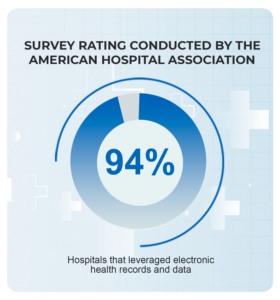
The changing needs of the industry have created an environment ripe for innovation. Consider that in 2019, the year before the pandemic, a survey conducted by the American Hospital Association found that 94% of hospitals leveraged electronic health records and data to perform processes that inform clinical practice. In other words, they use technology as a tool to better diagnose, treat, and care for patients.
The same survey found that hospitals also look to EHRs to identify patient care gaps, identify high-risk patients, support quality care improvement, monitor patient safety, and measure overall organization performance all at increasing rates.
Custom software systems developed for healthcare organizations are powerful tools for increasing communication and providing better patient care.
When technology, knowledge, and people work together, great things can be accomplished. The future of healthcare will be intertwined with technology and communication between patients and their care teams will benefit as a result.